Whilst recently observing teaching sessions at the University of Plymouth Faculty of Medicine & Dentistry, where the Simulated Patients play a major role, I had the opportunity to catch up with a number of our experienced Simulated Patients who work regularly in that location.
It was the first-year students’ first session with Simulated Patients and the students were working in pairs, each taking it in turns as a medical student role playing a scenario with a Simulated Patient, who would then, alongside their peer observer, give them feedback on their skills. Two facilitators were also circulating, keeping an eye on things and answering any questions that came up. It was great to see how much progress could be achieved in such intense work with students.
The University places a lot of trust in the Simulated Patients and I could see how much their input was valued. The students were, understandably, nervous and all the Simulated Patients did a great job in putting them at ease so they were able to learn.
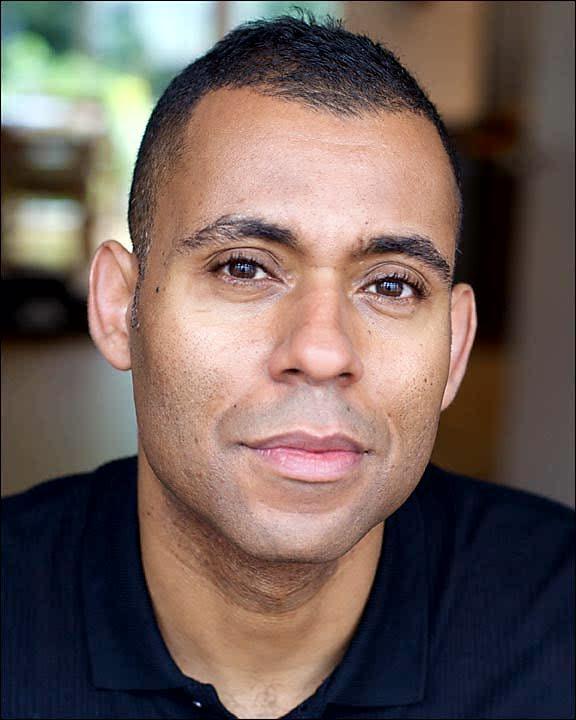
I spoke to one of the Simulated Patients, Neville Connor, afterwards, about his background and how he had decided to apply to Peel Roleplay to train to do this work. I had seen him firstly playing the role very realistically and then, in the feedback, picking out the details of the students’ strengths in communication and then, with great sensitivity, helping them – using a lot of open questions – to identify the areas that could be improved. “It helps to make them work and draw their own conclusions,” he said.
Most, but not all, Simulated Patients come from an acting background and whilst Neville has acting experience- he trained at Identity School of Drama in London and the International School of Screen Acting and has worked in theatre, film and television- he has had a varied career and was previously in the military.
Born and brought up in an inner-city part of Birmingham, he served in the Royal Logistics Corps or five years. “It taught me discipline, a strong work ethic and how to get on with things that I didn’t want to do,” he said. So how had he made the change from a military environment where – as he said – the ethos tended to be direct, matter of fact, “stick and carrot” and “Man up!” to helping medical students to improve their communication?
Now, Neville lives in Torquay and works for the NHS as a Senior Health Coach. He pointed out how times, and attitudes, are changing. “Communication and expressing yourself is a real strength”. Interpersonal skills, which were once known as “soft skills” and rather looked down upon, are now much more respected. “Soft skills are now the core skills,” he said.
Neville works on the MECC (Making Every Contact Count) programme which is an approach to behaviour change to help patients manage long-term conditions and illnesses. “Telling people what to do is not the most effective way to help them change”. He is also involved with the Connect 5 programme which is a mental health promotion training programme designed to increase the confidence and core skills of front line staff so they can be more effective in having conversations about mental health problems.
I could see how all the skills used in this work are directly transferable to working as a Simulated Patient and giving feedback to students. When I first met Neville, I felt that he intuitively understood the guiding principles of what it means to be a good Simulated Patient. The focus must always be on the students’ learning, development or assessment. It was great to see him putting this into practice.
I asked Neville how he was finding working with medical students. He said that it’s obvious how much they care about what they do and described them as “passionate and with a real sense of purpose”. He has found the standard of communication to be really high. Previously, medical students were often described as being arrogant but Neville says he has never come across this with today’s students. Neville believes that “lived experience” is a skill that is crucial to becoming a good Simulated Patient, working with student healthcare professionals from many different backgrounds.
What else can help?
“Never assume anything about anyone”.
By Laura Thompson, Simulated Patient Manager at Peel Roleplay